
Haemophilia A
Haemophilia A (HA; 2017 ICD-10-CM: D66) is an inherited bleeding disorder caused by the lack of coagulation factor (F) VIII activity. The F8 gene encodes for FVIII, which serves as a co-factor to FIXa in a complex that converts FX to the activated form FXa. As a result of this congenital deficiency, patients with HA have a defective clotting process and an increased tendency to bleed spontaneously and in response to traumatic injury. Replacement of the missing clotting factor is the standard treatment to prevent and control bleeding.
HA accounts for approximately 50% of all bleeding disorders and has a prevalence of approximately 1 per 5,000 live male births.1 The reported prevalence of HA differs depending on the economic status of a country.2,3 Globally, approximately 70% of patients with haemophilia are un- or misdiagnosed and untreated; the majority of these patients live in developing countries.3
The clinical manifestations of HA are prolonged and repeated bleeding episodes. Unless properly treated, haemorrhage into joints and muscles causes painful, progressive arthropathy and muscular atrophy,4 and can result in severe disability with vocational and psychological sequelae. While joints and muscles are the most common spontaneous bleeding sites,5 central nervous system bleeds are the leading causes of death in patients with haemophilia who are not infected with human immunodeficiency virus (HIV), accounting for approximately one-third of all deaths.6
HA is classified as 'mild', 'moderate' or 'severe' according to the residual activity of FVIII.5 Patients with mild HA may have severe bleeding during major trauma or surgery, but rarely have spontaneous bleeding. Patients with moderate HA experience occasional bleeding and prolonged bleeding with minor trauma or surgery. Severe HA is characterised by spontaneous bleeding into joints or muscles, predominantly in the absence of identifiable haemostatic challenge. Residual FVIII activity is generally expressed as a percentage of ‘normal’, which is variable between individuals and may range from 50–150%.7
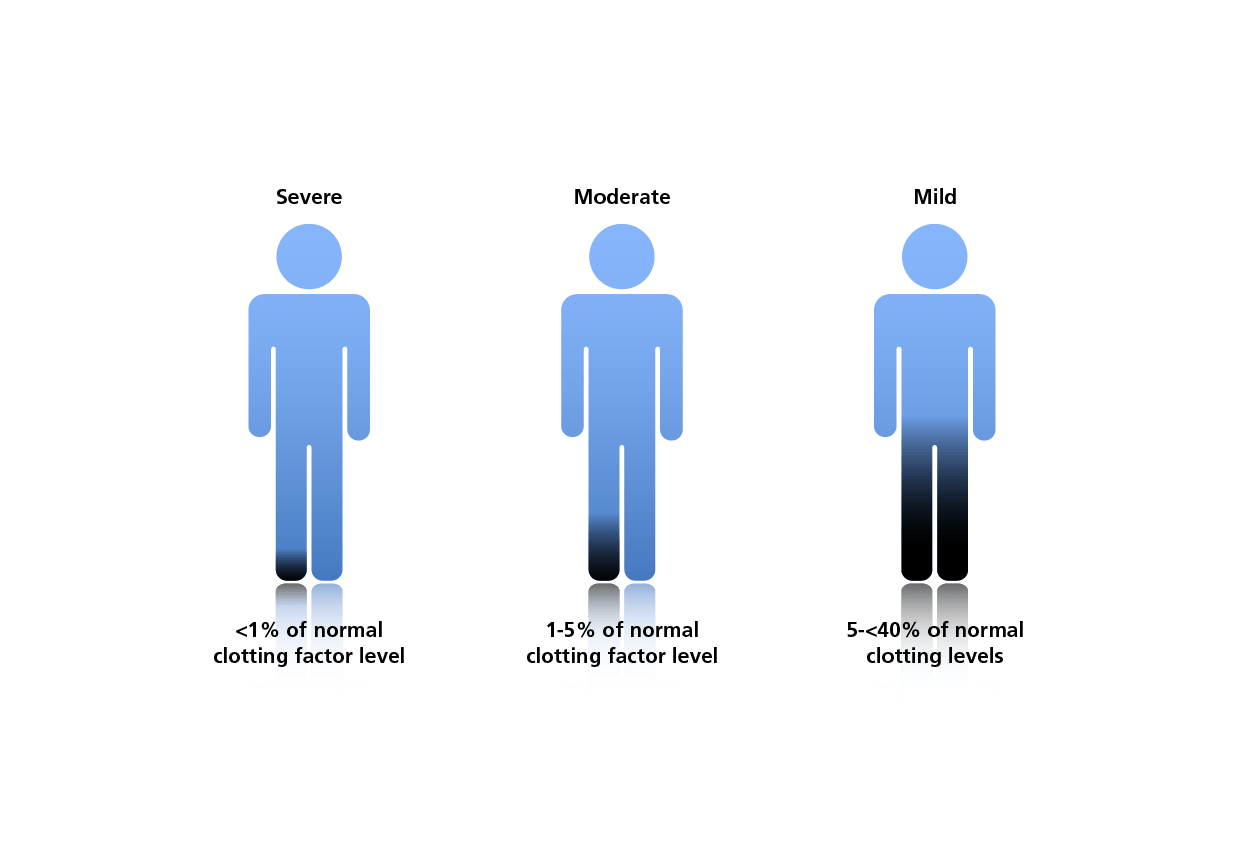
Classification of haemophilia A according to clotting factor levels5
HA is characterised by different underlying molecular defects affecting the F8 gene. Congenital haemophilia is inherited in an X-linked recessive manner and therefore largely affects men (although there are rare cases of females diagnosed with the disease). In approximately one-third of cases, however, there is no family history and haemophilia results from a spontaneous mutation.8 This balance between gene loss caused by low reproductive fitness and spontaneous mutation has sustained haemophilia within the general population. Female carriers may have decreased FVIII levels.9
A large number of gene mutations are known to affect clotting factor expression, including missense or nonsense mutations, defects in mRNA splicing, insertions and deletions. The CDC Hemophilia A Mutation Project (CHAMP) F8 Mutation List provides an overview of more than 2500 unique mutations identified to date for the F8 gene coding for FVIII.10
- Berntorp E, Shapiro AD. Modern haemophilia care. Lancet 2012; 379:1447-56.
- Stonebraker JS, Bolton-Maggs PH, Soucie JM, Walker I, Brooker M. A study of variations in the reported haemophilia A prevalence around the world. Haemophilia 2010;16:20-32.
- O'Mahony B, Black C. Expanding hemophilia care in developing countries. Semin Thromb Hemost 2005;31:561-8.
- Lottenberg R, Kentro TB, Kitchens CS. Acquired hemophilia. A natural history study of 16 patients with factor VIII inhibitors receiving little or no therapy. Arch Intern Med 1987;147:1077-81.
- World Federation of Hemophilia (WFH): Guidelines for the Management of Hemophilia; 2012.
- Darby SC, Kan SW, Spooner RJ, et al. Mortality rates, life expectancy, and causes of death in people with hemophilia A or B in the United Kingdom who were not infected with HIV. Blood 2007;110:815-25.
- Moser KA, Adcock Funk DM. Chromogenic factor VIII activity assay. Am J Hematol 2014;89:781-4.
- Hoyer LW. Hemophilia A. N Engl J Med 1994;330:38-47.
- Plug I, Mauser-Bunschoten EP, Bröcker-Vriends AHJT et al. Bleeding in carriers of hemophilia. Blood. 2006;108:52-6.
- Payne AB, Miller CH, Kelly FM, Michael Soucie J, Craig Hooper W. The CDC Hemophilia A Mutation Project (CHAMP) mutation list: a new online resource. Hum Mutat 2013;34:E2382-91.
HQMMA/NNG/0517/0163
